Submit Courtesy Claims with Ease Using Owl Practice Suite
File claims on behalf of your clients to make paying for therapy stress-free.
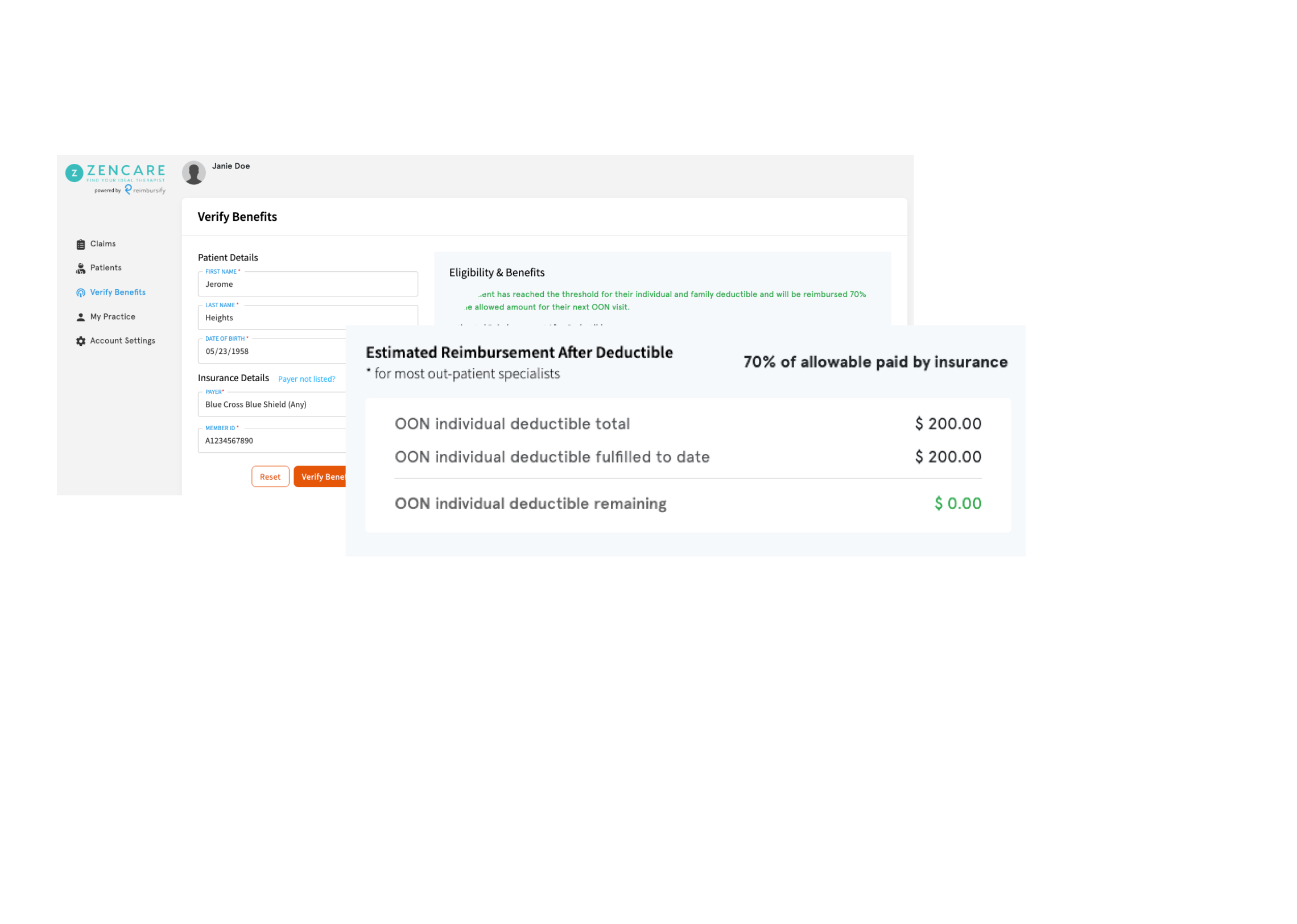
Help clients understand their costs.
With Instant out-of-network benefits checks you take-away the guesswork from the start.
Prospective clients can submit their insurance details within first contact and you can give them an estimate of how much they need to pay per session.
Clients who understand their out-of-network benefits are more likely to book first appointments because they know they can use their insurance benefits to offset costs.
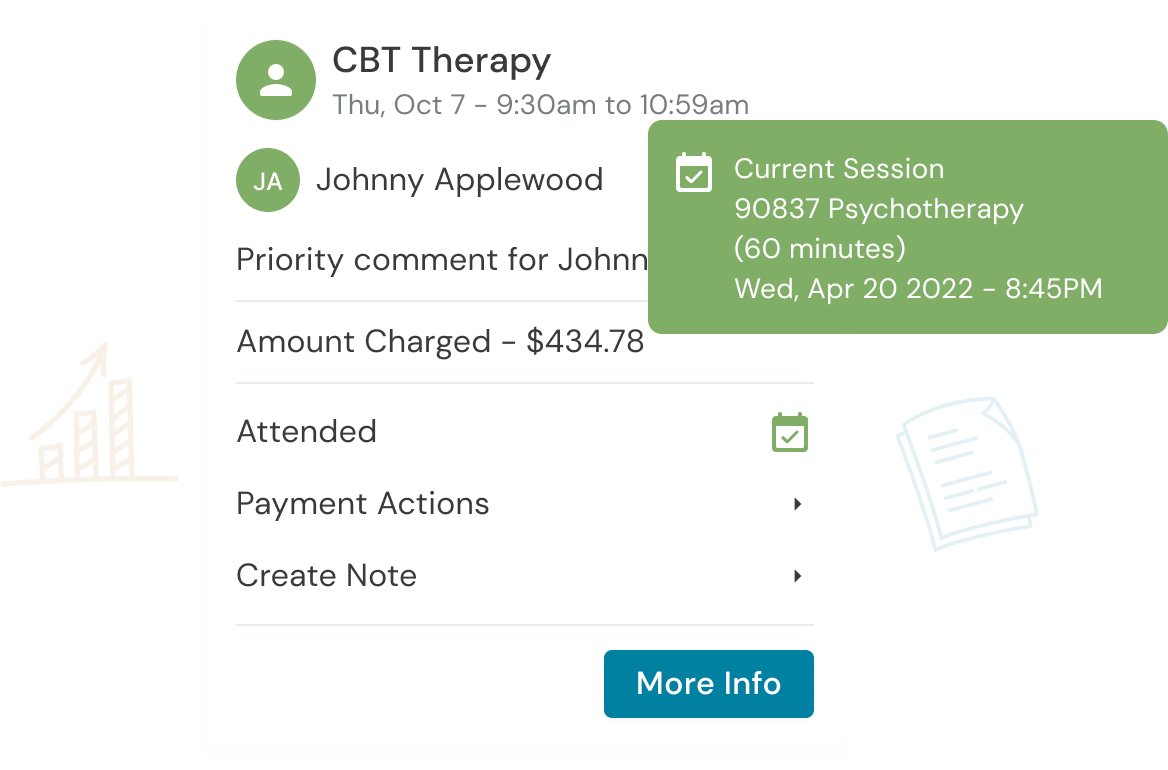
Make sure your clients get reimbursed
Clients who get reimbursed miss fewer sessions and stay in therapy longer.
File claims on behalf of your clients to help make paying for therapy stress-free
Clients who get reimbursed are more satisfied, miss fewer sessions, and stay in therapy longer – meaning better client retention and more stable practice revenue
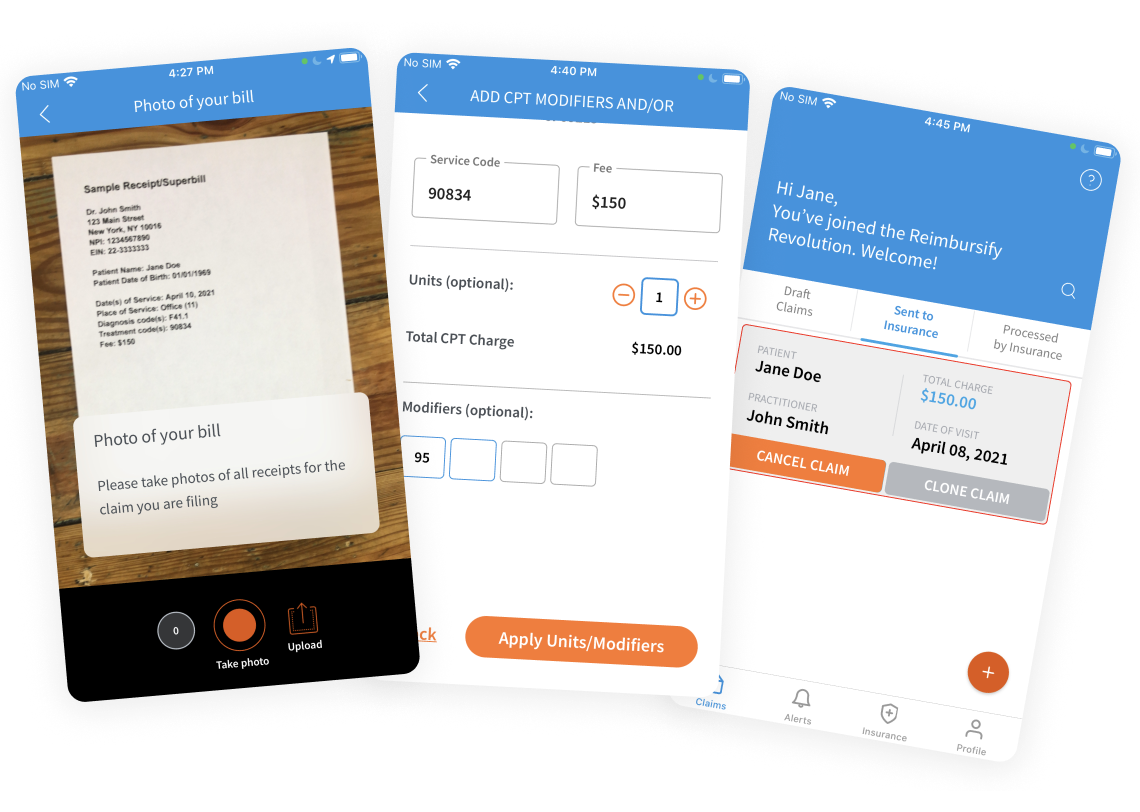
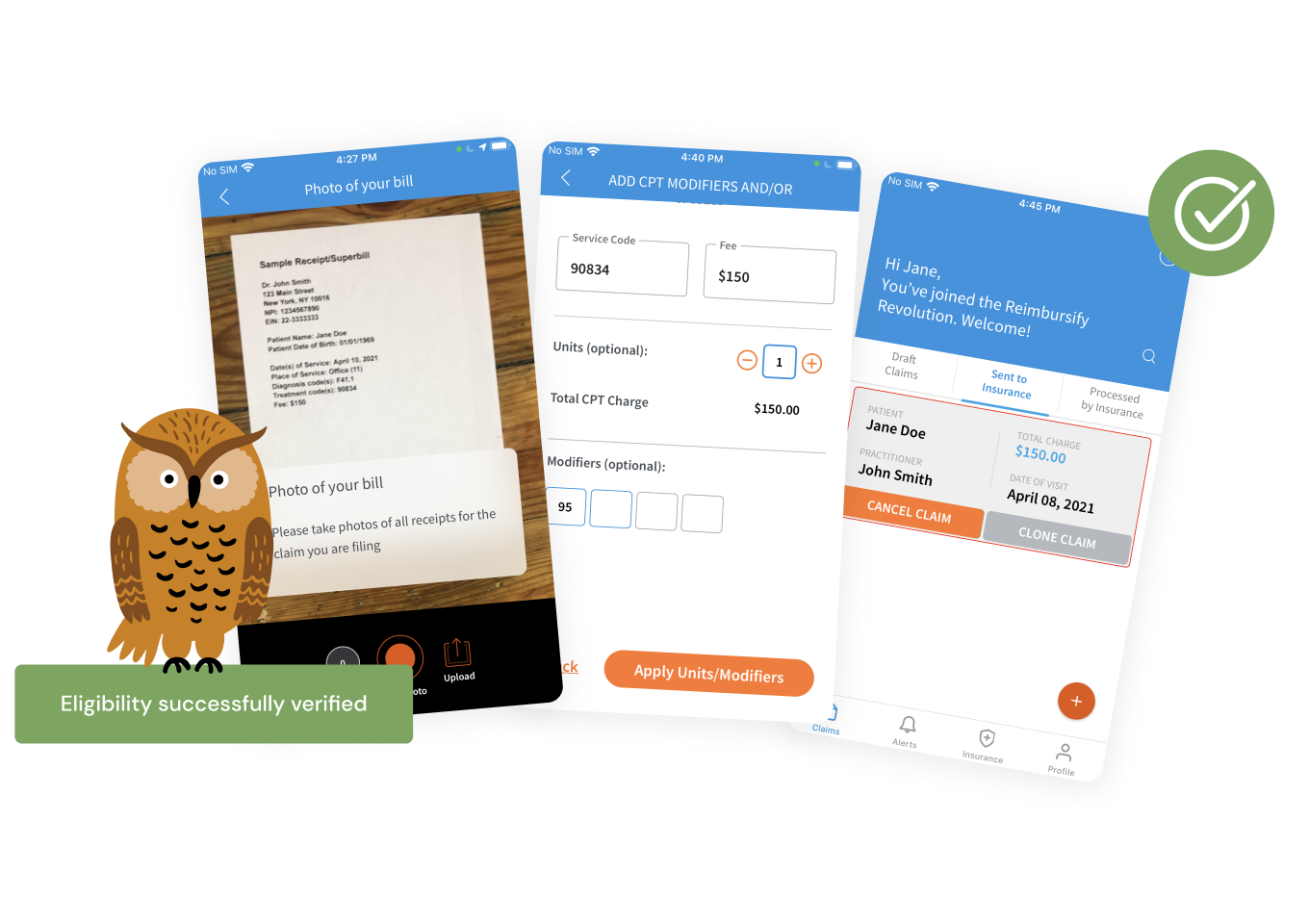
Empower clients to manage their claims
Clients can file their claims for free using our easy-to-use mobile app when you add-on courtesy claims.
Our accompanying app dramatically simplifies the entire claim submission process by allowing clients to submit, track, and manage their therapy claims
It’s easy to use, with regular claim status updates , so clients never have to remember to follow up
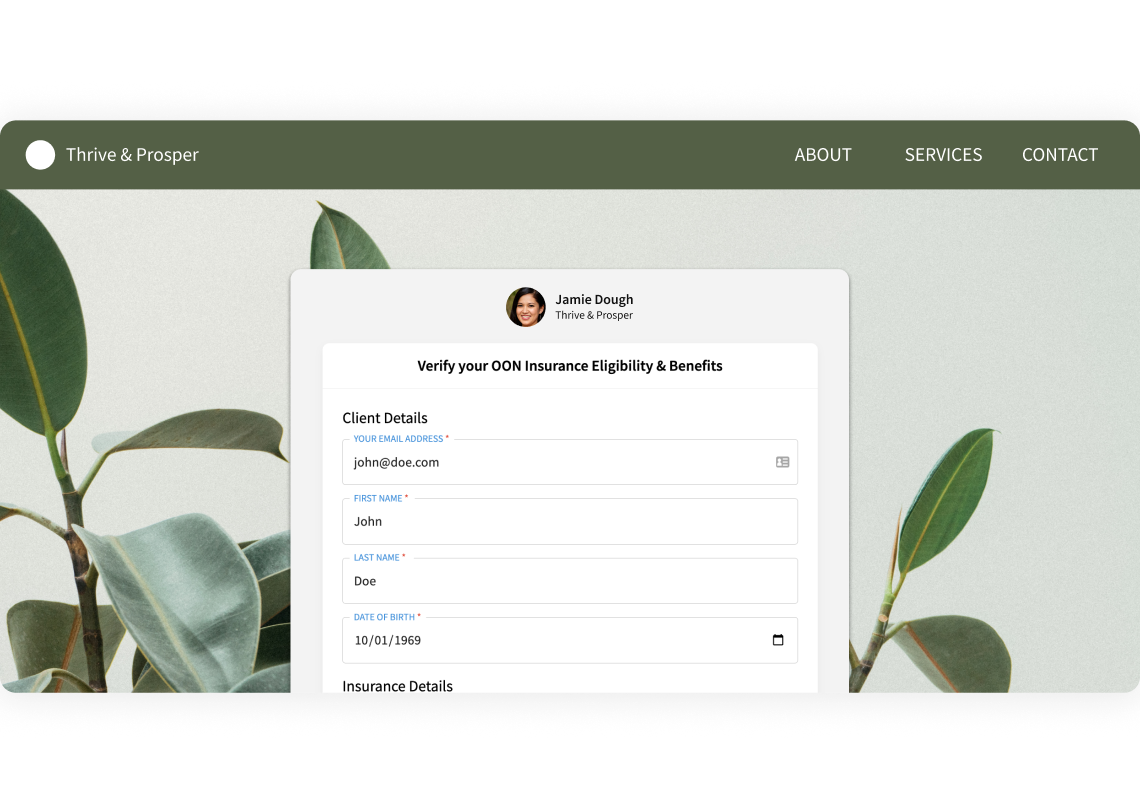
Give clients the tools they need right on your website
Our plug-in makes it easy for clients to verify their benefits and file claims directly on your practice website.
Your clients can file their own claims and verify their out-of-network benefits without leaving your site!
The widget is incredibly simple to add to your page, but if you have any issues, our customer support team can easily help you add it.
Join the thousands of therapists using Owl to run their practice every day.
Frequently Asked Questions
Clients will be able to see the estimated cost of your service. The deductible will be hidden, as will the amount they have paid towards it so far. If they consent, this information can be sent to you directly so you can have a detailed conversation with them about the cost of your services.
Our digitized process delivers claims to insurance payers’ processing hubs within hours. While many payers process the claims within a week or two, we recommend allowing four to six weeks for processing (since that is a time frame stipulated by most states.
Sign up for Practice Wisdom. Tips to help your practice thrive.