Save your time and your sanity.
Our fully integrated electronic insurance claims get you paid faster.
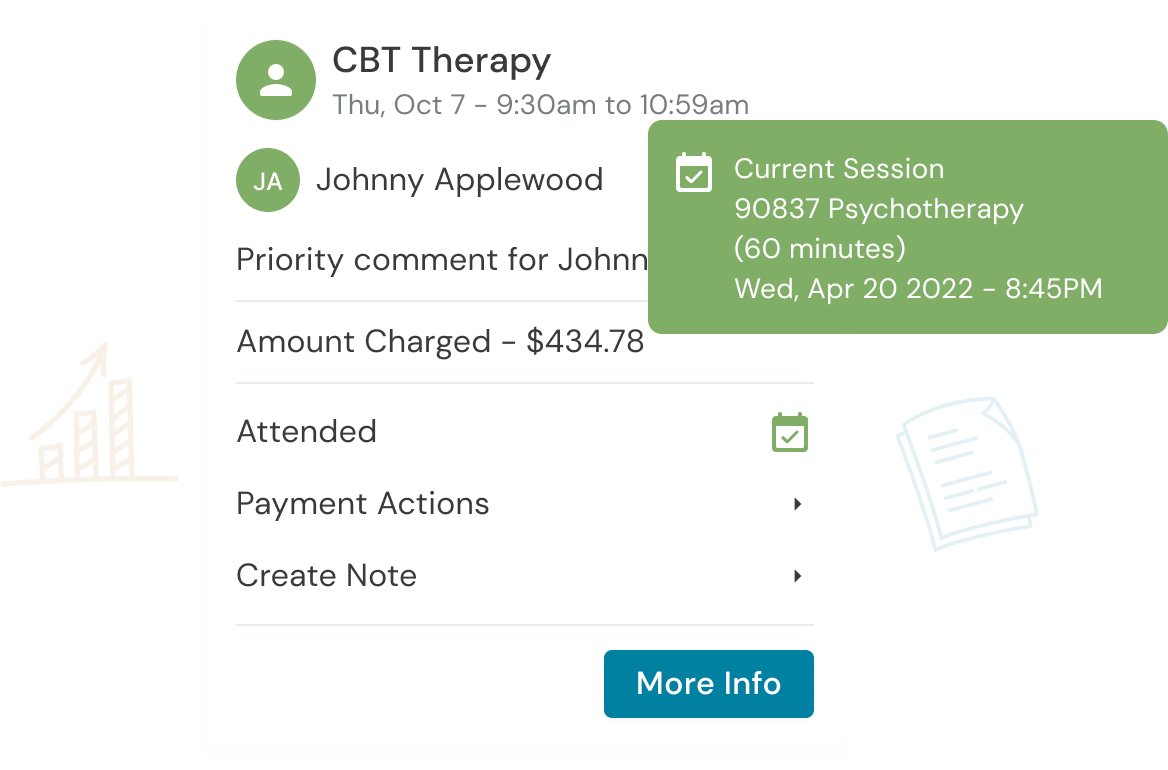
Manage all tasks related to creating, submitting, and tracking insurance claims within Owl
There is no need to manually enter data – your practice and client data automatically fill the claims – making the whole process take seconds
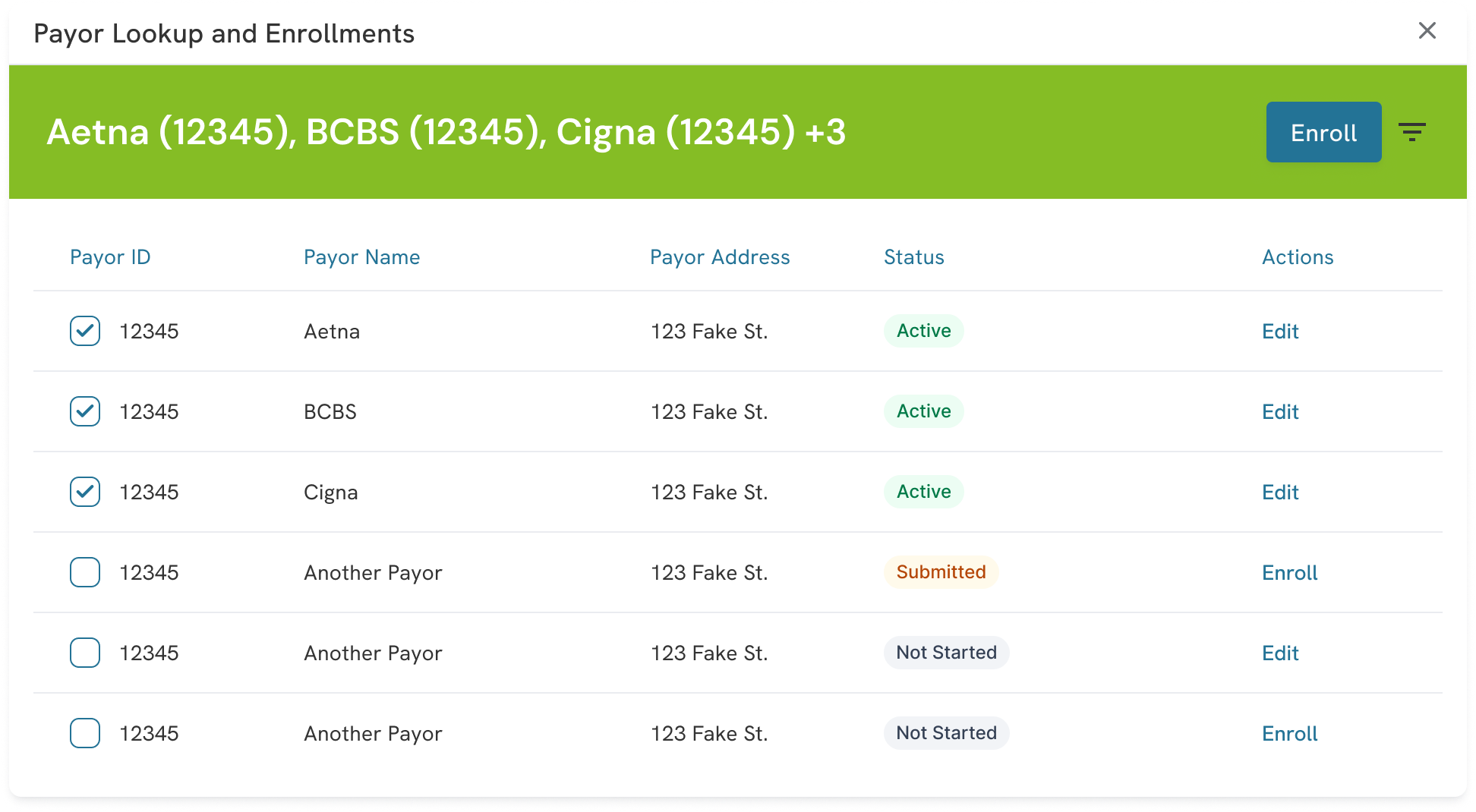
Enroll with payers with ease.
Let us do the heavy lifting of payor enrollment – with no extra charge.
Enroll with all your payers right in Owl, and be automatically notified as soon as you are approved
Simply submit the request and our team handles the rest. No back and forth with the insurance companies is necessary
Spend less time making calls to insurance
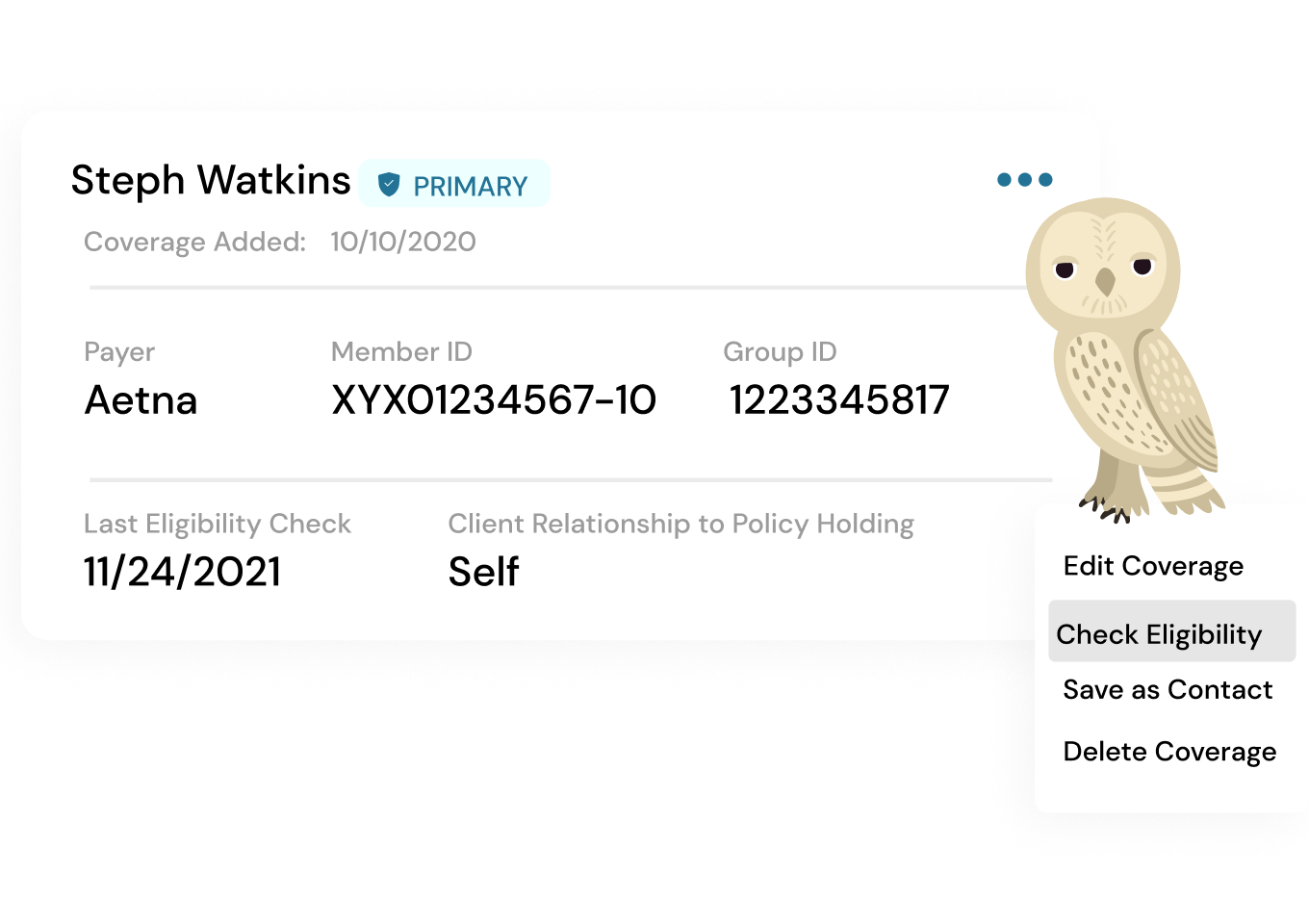
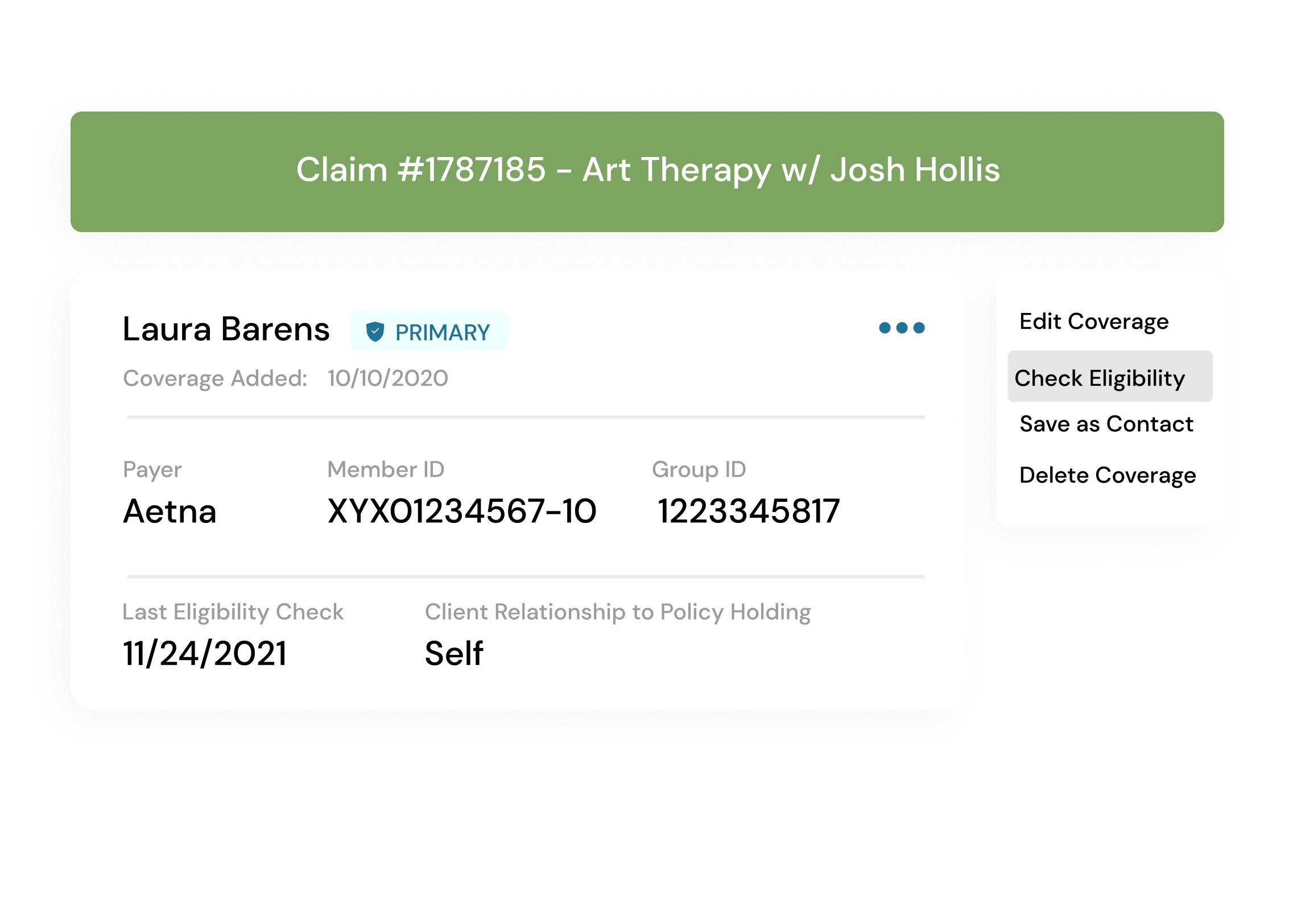
Verify your clients’ coverage in a click
Add client coverage directly in their profile and manage multiple plans if applicable
Verification of benefits reports provides your clients with important, up-to-date information about their copay and deductible.
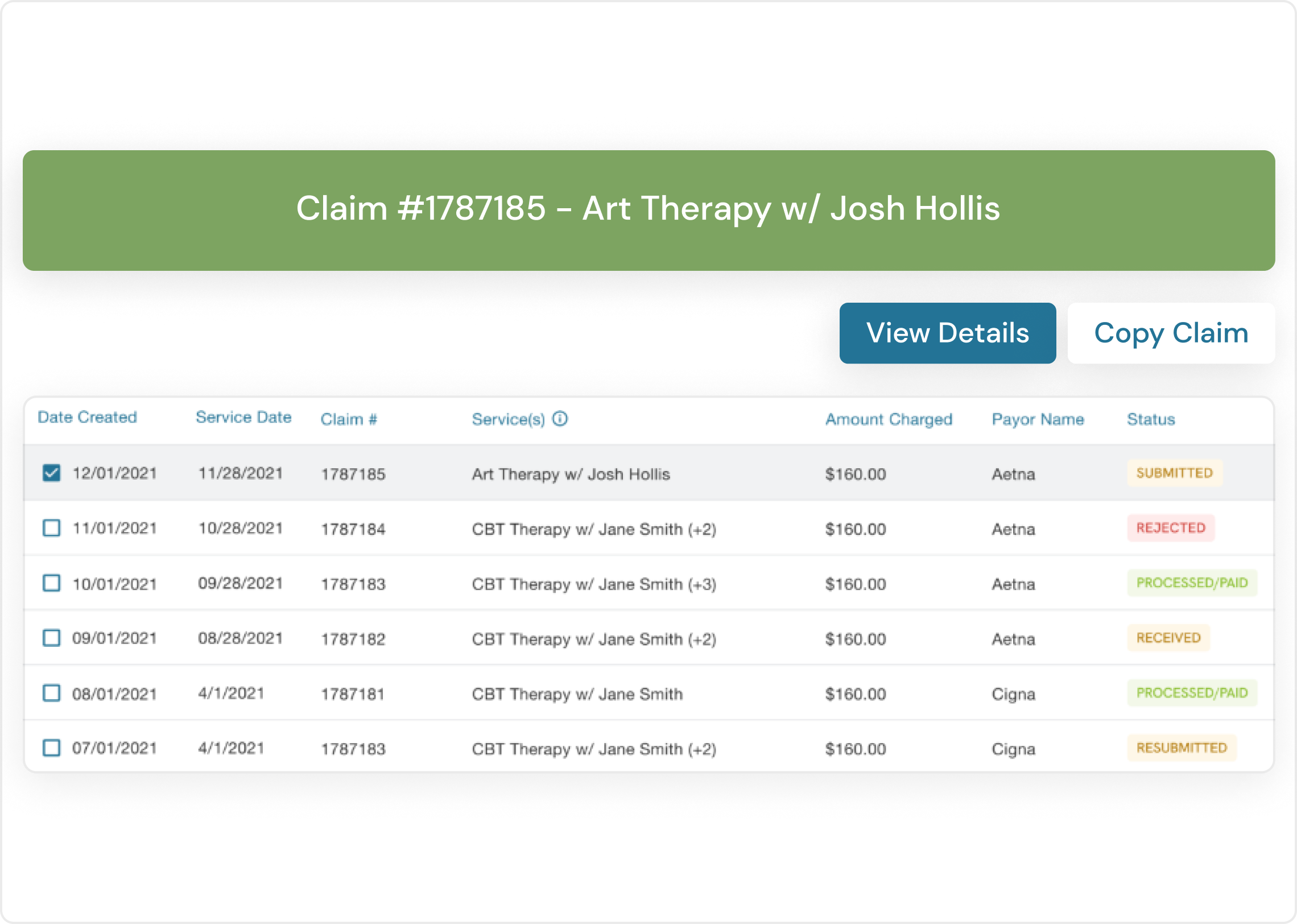
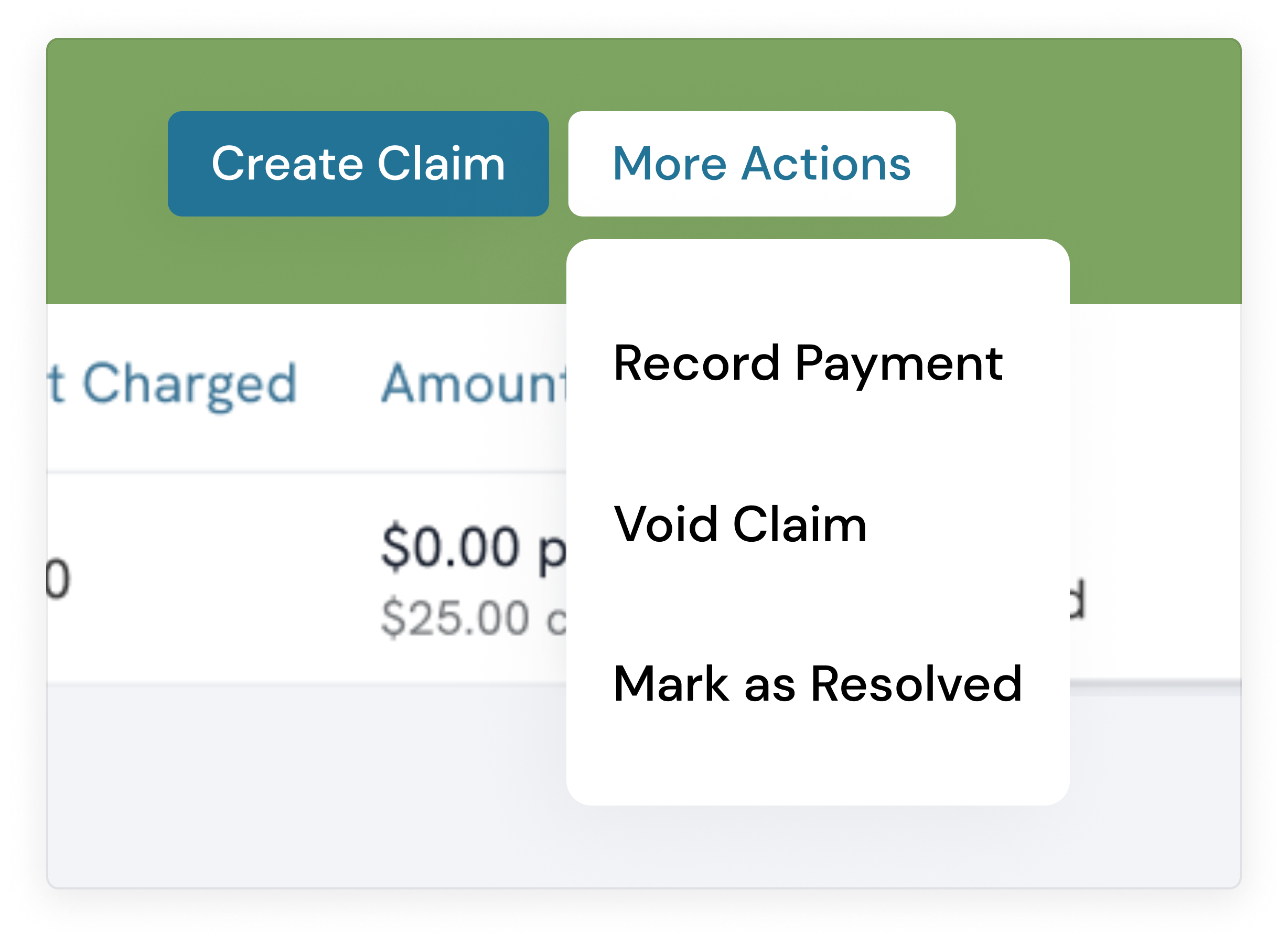
Get paid faster
Reduce rejections with better claim accuracy and tools to bring important tasks to your attention.
Enjoy seamless client invoicing for unpaid portions and co-pays
Submit claims to over 5,000 payers seamlessly with minimal effort. Benefit from detailed insights into claim rejections and quickly revise and resubmit claims to ensure prompt payments.
Stay in the loop with real-time claim status tracking and alerts

We have been very happy with the results from Zencare with Private Pay Booster. We have been able to convert almost all OON prospects who have used the checker into clients!

Private Pay Booster has led to increased patient contacts —they appreciate having an idea of insurance reimbursement rates for private pay sessions at the time of contact!
Join the thousands of therapists using Owl to run their practice every day.
Frequently Asked Questions
Enrolling is easy with Owl! Simply set up your insurance profile within the Owl application. Select the in-network insurance companies you work with, and our team will handle the rest. You’ll be enrolled for electronic claims with all your in-network insurers without any hassle.
Claim rejections can be frustrating, but Owl makes it easy to address them. Our system leverages accurate data from your client’s chart and industry-best practices to minimize rejection risks. If a claim is rejected, Owl instantly updates the claim status in the system and provides the specific error or rejection reason. You can then correct the issue and resubmit the claim with just a few clicks. We’re dedicated to helping you get paid for all eligible claims with minimal complexity.
Some claims are paid in as few as two days, with the majority settling within ten days.
Sign up for Practice Wisdom. Tips to help your practice thrive.