Understanding the terminology of mental health billing is essential for therapists and their administrative staff to navigate the often-complex world of insurance and payments. This comprehensive glossary provides clear definitions of key terms, from CPT codes to eligibility verification, empowering mental health professionals to manage their billing processes with confidence and efficiency. Whether you’re new to billing or seeking a quick reference guide, these terms will help streamline your practice’s administrative tasks and improve overall accuracy.
CPT Code (Current Procedural Terminology Code)
A code used to describe specific medical procedures and services provided by mental health therapists, such as psychotherapy sessions.
ICD-10 Code (International Classification of Diseases, 10th Edition)
A diagnostic code used to identify and categorize mental health conditions and disorders for insurance billing and medical records.
CMS-1500 Form
The standard claim form used for submitting insurance claims for healthcare services, including mental health therapy.
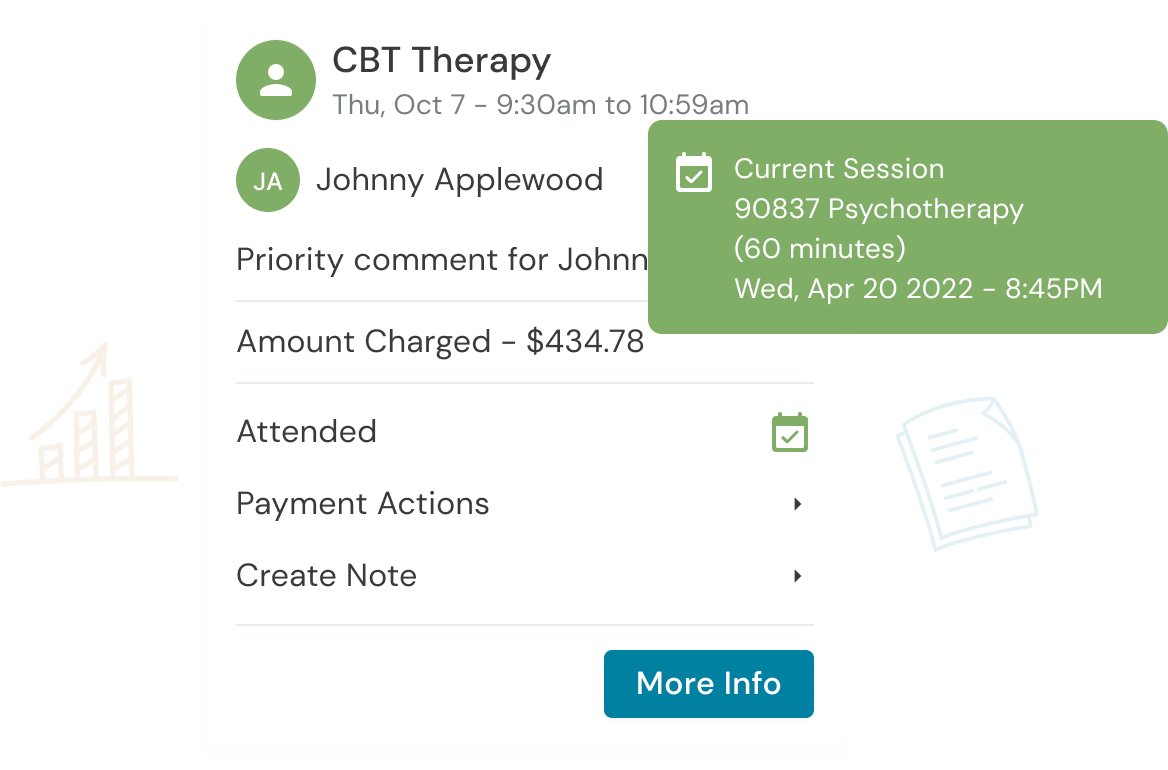
Superbill
A document that summarizes the services provided during a client’s visit, including CPT codes, ICD-10 codes, and other relevant information, for insurance billing purposes.
Eligibility Verification
The process of checking a client’s insurance coverage to determine if they are eligible for mental health services, including coverage, co-pays, and deductibles.
Prior Authorization
A requirement by some insurance companies to obtain approval before providing specific mental health services. It ensures that the service is deemed medically necessary.
EOB (Explanation of Benefits)
A document sent by an insurance company to explain the details of a claim’s payment or denial, including services covered, payments made, and client responsibilities.
NPI (National Provider Identifier)
A unique 10-digit identifier for healthcare providers, including mental health therapists, used for billing and claims processing.
Clearinghouse
A third-party service that processes and submits insurance claims on behalf of healthcare providers, improving accuracy and efficiency in the billing process.
Client Responsibility
The portion of a mental health service cost that the client is responsible for paying, which includes co-pays, deductibles, and coinsurance.
Claim Rejection
When an insurance company refuses to process a submitted claim due to errors, inaccuracies, or other issues, requiring correction and resubmission.
Claim Denial
A decision by the insurance company to refuse payment for a mental health service, often due to lack of medical necessity, non-covered services, or policy violations.
Billing Modifier
A code added to a CPT code to provide additional information about the service, such as the time spent or the specific circumstances of the therapy session.
Clean Claim
A correctly completed claim that contains all necessary information and adheres to insurance company requirements, making it more likely to be processed without issues.
Payer
The entity responsible for providing payment for mental health services, such as an insurance company or a government agency like Medicaid or Medicare.
CMS (Centers for Medicare & Medicaid Services)
A federal agency that oversees
Medicare, Medicaid, and other healthcare programs in the United States, setting billing and reimbursement rules.
Coordination of Benefits (COB)
A process that determines how multiple insurance policies covering a client should work together to pay for mental health services.
Coinsurance
The client’s share of the costs for a mental health service after the deductible has been met, typically
represented as a percentage of the service cost.
Medically Necessary
A term used to indicate that a mental health service is essential for the treatment and well-being of a client and, therefore, should be covered by insurance.
EHR (Electronic Health Record)
Digital records of a client’s mental health history, treatment, and billing information, often used for accurate billing and record-keeping.
Overpayment
An excess payment made by an insurance company for a mental health service, which may need to be returned or adjusted in future claims.
Get the “Ultimate Guide to Navigating Insurance” eBook Below!
Reduce clinical administrative tasks and transform more lives with Owl Practice. Owl Practice provides all the tools you need to make your practice successful. Join the thousands of care professionals using Owl to run their practice every day.