Deciding to accept out-of-network insurance coverage can open new opportunities for mental health practitioners, allowing them to serve a broader client base and enhance their practice’s financial health.
This involves understanding two billing methods: using a superbill and offering courtesy billing. By leveraging these methods and understanding billing and reimbursement practices, therapists can create a successful, financially sound practice that reaches a wider clientele.

Leveraging Out-of-Network Insurance Coverage
For mental health therapists, the decision to accept out-of-net- work insurance coverage can open up new opportunities. While it comes with different challenges compared to being in-network, leveraging out-of-network insurance coverage can be a strategic move to serve a broader client base and enhance the financial health of your practice.
Below, we’ll explore how mental health therapists can effectively utilize out- of-network insurance coverage.
The Benefits of Accepting Out-of-Network Insurance
For mental health therapists, the decision to accept out-of-network insurance coverage can open up new opportunities. While it comes with different challenges compared to being in-network, leveraging out-of-network insurance coverage can be a strategic move to serve a broader client base and enhance the financial health of your practice.
Expanded Client Base: Accepting out-of-network insurance allows you to work with clients who have insurance plans that you are not in-network with.
More Pay Per Client: Working with an out-of-network client means that you can charge your self-pay rate to the client, and the client will pay the full fee up front. If the client has out-of-network benefits, then their insurance can reimburse them a percentage of the self-pay rate.
Client Flexibility: Clients may appreciate the option to see a therapist of their choice, even if you are out-of-network, and are willing to pay the difference.
Understanding Out-of-Network Benefits
Treatment Guidelines: Before accepting a new client, verify their out-of-network benefits. This includes understanding their deductible, co-payment, and maximum allowable amount.
Claim Submission: Educate your clients about the process of submitting claims to their insurance company. Ensure they keep records of sessions and receipts for reimbursement.
Billing and Reimbursement
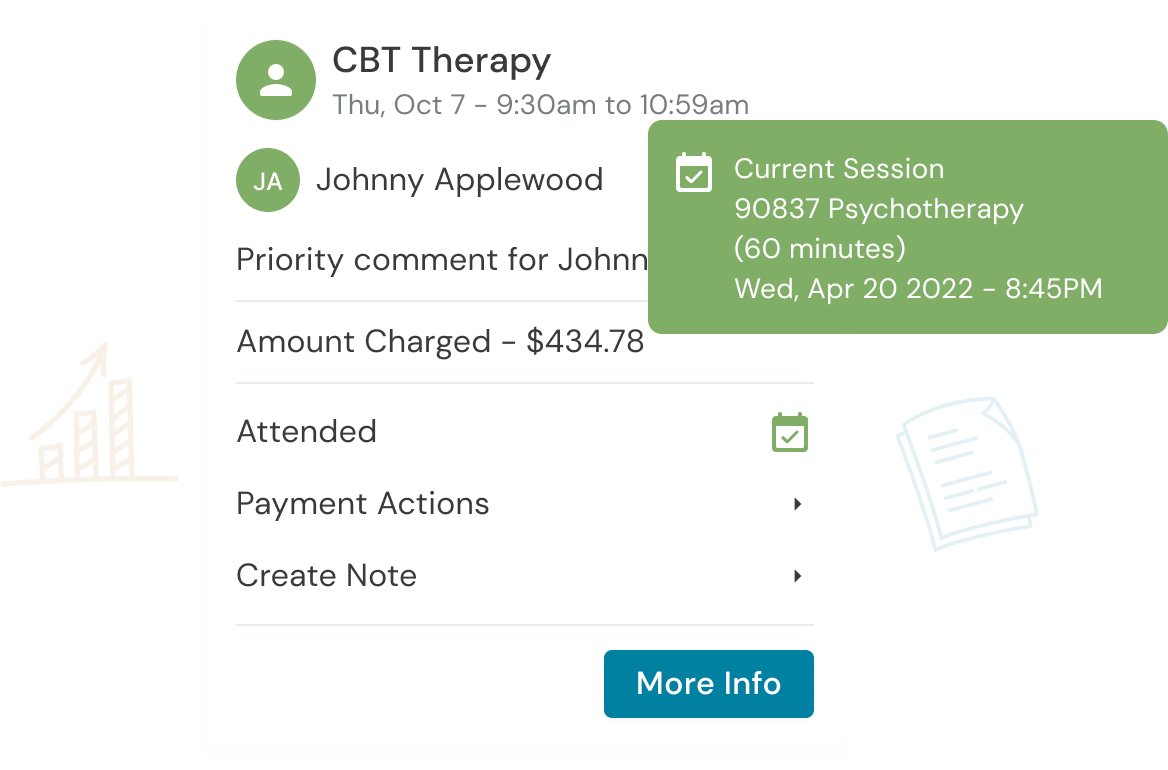
Superbills: Provide clients with superbills, which are detailed invoices that they can submit to their insurance companies for reimbursement.
Billing Transparency: Clearly outline your fees and billing practices to clients from the beginning, ensuring they understand the financial aspect of out-of-net- work therapy.
W-9 Form: Insurance companies will want a W-9 form from you, even if you are an OON provider.
Effective Communication
Open Dialogue: Maintain transparent and open communication with your clients regarding their insurance coverage and financial responsibilities.
Educate Clients: Help clients understand how out-of-network coverage works and the steps they need to take to seek reimbursement.
Navigating Administrative Challenges
Documentation: Accurate and thorough record-keeping is crucial. Ensure that your session notes are comprehensive to support claims.
- Helpful Tip: Laissez-faire about notes? Don’t be. If you are audited, the insurance company will clawback from the client if your records do not meet medical necessity.
Timely Filing: Familiarize yourself with the insurance company’s filing deadlines to ensure claims are submitted promptly.
Good Faith Estimate: This is a provision of the No Surprises Act where a provider must give clients an estimate of how much they will be charged for the therapy sessions they will be receiving. As of January 1, 2022, if you are a state-licensed or certified health care provider, you are required to give a Good Faith Estimate to every new and continuing client who is either uninsured or is not planning to submit a claim to their insurance for the sessions they have with you.
Strategies to Attract Out-of-Network Clients
Marketing: Promote your out-of- network services through your website, social media, and therapist directories to attract clients seeking specialized care.
Specializations: Highlight your expertise and unique therapeutic approaches to appeal to clients willing to
invest in out-of-network services.
Provide VOB Insights: Using a tool like Owl Practice Suite’s Verification of Benefits tool on your website can allow clients to look up their benefits coverage prior to booking an appointment. Therapists with a tool like this on their website see a 50% increase in their first appointments booked.
Managing Client Expectations
Discuss Expectations: Clearly communicate to clients that while you are out-of-network, you offer
specialized and high-quality services that may be worth the additional investment.
Sliding Scale: Consider offering a sliding scale or payment plans for clients who may struggle to pay your full fee.
Summary
Leveraging out-of-network insurance coverage can be a valuable strategy for mental health therapists. By understanding the benefits, effectively communicating with clients, and navigating the administrative aspects of billing, you can create a successful practice that reaches a wider clientele.
In doing so, you not only offer your expertise to those who need it but also maintain a thriving and financially sound mental health therapy practice.
Get the “Ultimate Guide to Navigating Insurance” eBook Below!
Reduce clinical administrative tasks and transform more lives with Owl Practice. Owl Practice provides all the tools you need to make your practice successful. Join the thousands of care professionals using Owl to run their practice every day.