In the realm of therapy, documentation like SOAP notes isn’t just a formality—it’s a critical component of effective client care. Among the various methods available, SOAP notes stand out as a standardized and highly effective approach for recording client interactions. Whether you’re a seasoned therapist or new to private practice, mastering SOAP notes can significantly enhance your practice, ensuring continuity of care, legal protection, and efficient management.
Understanding SOAP Notes for Therapists
SOAP notes are a structured method for documenting client sessions, ensuring that important details are recorded in a consistent and organized manner. The acronym SOAP stands for:
- S (Subjective): This section captures the client’s perspective, including their feelings, concerns, and experiences as described in their own words. This is an opportunity for the therapist to document the client’s subjective experience, which can provide valuable insights into the client’s internal state and help guide the overall treatment plan.
- O (Objective): Here, the therapist records observable data such as the client’s behavior, mood, and physical appearance during the session. This section is focused on factual observations rather than interpretations, allowing the therapist to build a clear and objective record of the client’s presentation.
- A (Assessment): This part involves the therapist’s clinical interpretation based on subjective and objective information. It includes diagnoses, progress notes, and any clinical impressions. The assessment section allows the therapist to synthesize the information gathered and provide a professional evaluation of the client’s condition, progress, and any necessary adjustments to the treatment plan.
- P (Plan): The final section outlines the future course of treatment, including planned interventions, homework assignments, and the scheduling of future sessions. This section is crucial for ensuring continuity of care and keeping the client and any other healthcare providers informed about the next steps in the therapeutic process.
Each component of SOAP notes plays a vital role in creating a comprehensive record of the client’s journey through therapy. By consistently following this structured approach, therapists can ensure that important details are not overlooked, and that the client’s progress and care are thoroughly documented.

Get Your Free SOAP Note Template Now!
Why SOAP Notes Are Essential for Therapists
SOAP notes are more than just a way to keep track of what happens in a session—they’re a key tool for ensuring that your clients receive the best possible care. Here’s why they matter:
- Continuity of Care: SOAP notes provide a clear and detailed record of each session, making it easier to track progress over time and ensuring that any therapist who reviews the notes can understand the client’s history and treatment plan. This is especially important in cases where a client works with multiple therapists or if a therapist takes over a client’s care from a colleague.
- Legal and Ethical Protection: Detailed and accurate notes are essential for protecting both the therapist and the client. They can serve as legal evidence if there are any disputes or legal issues down the road, and they also demonstrate that the therapist is upholding their ethical responsibilities by maintaining thorough records.
- Treatment Planning: SOAP notes help in developing and adjusting treatment plans based on ongoing assessments of the client’s progress. By carefully documenting the client’s subjective experiences, the therapist’s observations, and the clinical impressions, they can make informed decisions about the most effective interventions and modifications to the treatment approach.
- Collaboration: If the client is working with multiple healthcare providers, SOAP notes ensure that everyone involved in the client’s care is on the same page. This promotes better coordination of treatment and allows for more effective collaboration among the various professionals involved in the client’s wellbeing.
How to Write Effective SOAP Notes for Therapists
Writing SOAP notes might seem daunting at first, but with practice, it becomes second nature. Here’s how to tackle each section:
S (Subjective)
Start by documenting the client’s perspective. This includes their thoughts, feelings, and any relevant history they share during the session. The subjective section is focused on capturing the client’s own words and experiences, which can provide valuable insight into their internal world and the challenges they are facing.
- Example: “The client reports feeling anxious about their upcoming job interview, stating, ‘I haven’t slept well all week because I’m so nervous.’”
O (Objective)
Next, record your observations. This section should be factual and devoid of interpretation. Focus on what you can observe directly—such as the client’s demeanor, body language, or any notable changes in their physical appearance. The objective section is about describing the client’s outward presentation without making any judgments or assumptions.
- Example: “The client appeared restless, frequently tapping their foot and avoiding eye contact.”
A (Assessment)
Here, synthesize the information from the subjective and objective sections into a clinical assessment. This might include a diagnosis, a discussion of the client’s progress, or any changes in their symptoms. The assessment section allows the therapist to provide a professional evaluation of the client’s condition and the overall trajectory of the treatment.
- Example: “The client’s anxiety appears to be escalating, as evidenced by increased restlessness and sleep disturbances. Anxiety Disorder remains the primary diagnosis.”
P (Plan)
Finally, outline the next steps in the client’s treatment. This could involve setting goals for the next session, assigning homework, or deciding on future interventions. The plan section is crucial for ensuring that the client’s care remains consistent, and that the therapist and the client are both on the same page about the next steps in the therapeutic process.
- Example: “Continue CBT techniques for anxiety management, explore possible medication referral if symptoms persist, and schedule follow-up in one week.”
SOAP Notes Examples
To help solidify your understanding of SOAP notes, here are a couple of examples based on common client scenarios:
Case Example 1: Anxiety Disorder
- S: “The client reports ongoing anxiety about social situations, stating, ‘I feel like everyone is judging me whenever I walk into a room.’”
- O: “The client displayed signs of nervousness during the session, including fidgeting and avoiding eye contact.”
- A: “Symptoms consistent with Social Anxiety Disorder. The client is beginning to apply CBT strategies but requires further practice.”
- P: “Increase exposure exercises in therapy, assign weekly social challenges, and schedule the next session in two weeks.”
Case Example 2: Depression
- S: “The client reports feeling ‘numb’ and ‘disconnected’ from everyday life.”
- O: “Client presented with a flat affect, spoke in a monotone voice, and had poor eye contact.”
- A: “Signs point towards moderate depressive symptoms. The client’s lack of engagement indicates a potential need for medication evaluation.”
- P: “Discuss possible medication options with the client, continue supportive therapy, and reassess in two weeks.”
These examples illustrate how SOAP notes can be used to create a clear, concise, and actionable record of each session, ensuring that client care is both effective and well-documented.
Best Practices for Maintaining SOAP Notes
To get the most out of SOAP notes, it’s important to follow some best practices:
- Consistency: Ensure that you document notes consistently after each session. This helps maintain a complete and continuous record of the client’s progress and treatment.
- Objectivity: Stick to the facts, especially in the Objective section. Avoid letting personal biases or interpretations influence your notes. The goal is to provide a neutral and accurate account of the client’s presentation.
- Clarity: Write notes that are clear and easy to understand. Avoid jargon or abbreviations that might confuse others who read the notes, such as other healthcare providers or legal professionals.
- Legal Considerations: Keep in mind the importance of privacy and confidentiality. Store your notes securely and ensure they comply with HIPAA regulations and any other relevant laws or ethical guidelines.
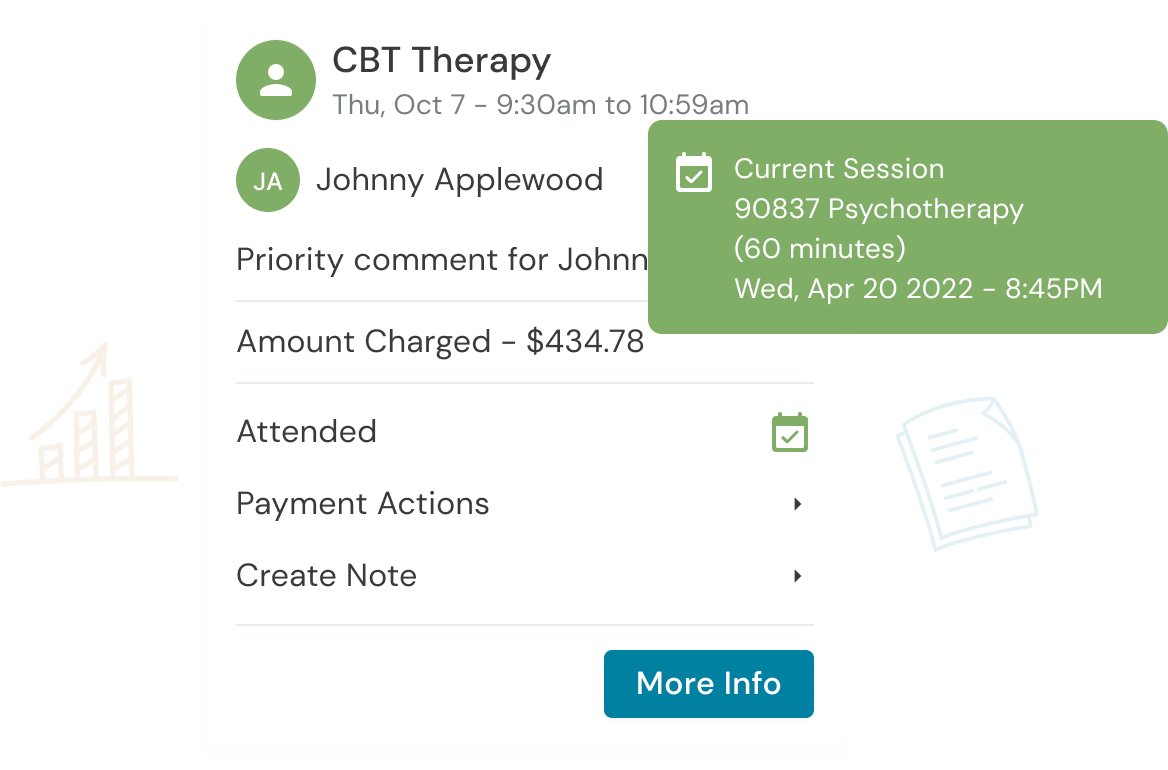
One way to streamline the note-taking process is by using an Electronic Health Record (EHR) system like Owl Practice, which offers tools specifically designed for mental health professionals. With features that help ensure compliance, efficiency, and security, Owl Practice can simplify the process of maintaining SOAP notes, allowing you to focus more on client care. Owl Practice’s EHR includes a SOAP note template, along with other note templates for your practice. You can also handwrite notes if you prefer that approach.
FAQ: Common Questions About SOAP Notes
Q: What are SOAP notes in therapy?
A: SOAP notes are a standardized method for therapists to document client sessions, ensuring important details are recorded consistently. The SOAP acronym stands for Subjective, Objective, Assessment, and Plan.
Q: How do SOAP notes protect therapists legally?
A: Detailed SOAP notes can serve as legal evidence, offering protection in case of disputes or legal issues, ensuring that the therapist has an accurate record of each session. They demonstrate that the therapist is upholding their ethical responsibilities and providing appropriate care.
Q: What are some best practices for writing SOAP notes?
A: Consistency, objectivity, and clarity are key. Ensure that notes are written immediately after sessions, stick to the facts, and avoid jargon or unnecessary abbreviations. Additionally, maintain secure storage and compliance with relevant laws and regulations.
Conclusion
SOAP notes are a vital part of the therapeutic process, ensuring that your client’s journey is well-documented and that your practice runs smoothly. By mastering this method, you not only enhance your clients’ care but also protect yourself and your practice from potential legal and ethical issues. Whether you’re new to SOAP notes or looking to refine your approach, consistency, objectivity, and clarity are key.
At Owl Practice, we’re here to help you manage your practice more efficiently. Our EHR system is designed to streamline the documentation process, making it easier for you to maintain thorough and accurate records. Ready to improve your documentation? SOAP Notes are a pre-loaded notes template option in Owl Practice!
Reduce clinical administrative tasks and transform more lives with Owl Practice. Owl Practice provides all the tools you need to make your practice successful. Join the thousands of care professionals using Owl to run their practice every day.